13
Mar 2024
Pediatric CPR: Adapting Techniques for Younger Individuals
Published in General on March 13, 2024
Pediatric CPR, or cardio-pulmonary resuscitation, plays a critical role in saving lives and helping to maintain the well-being of younger individuals. It is essential for caregivers, parents, teachers, and anyone who interacts with children to be familiar with the basics of pediatric CPR. By understanding how to adapt CPR techniques for younger individuals, you can increase the chances of successful resuscitation in an emergency situation.
1. Understanding Pediatric CPR Basics:
Performing pediatric CPR requires a solid foundation in basic life support (BLS) techniques. However, it is important to note that there are some differences when administering CPR to children compared to adults. The first key difference is the compression-to-ventilation ratio. For adults, it is typically 30 compressions followed by two breaths. In pediatric cases (children aged 1 to puberty), the recommended ratio shifts to 30 compressions followed by one breath. Signing up for courses offered by companies like TinyHearts can help parents familiarise themselves with the essentials of pediatric CPR.
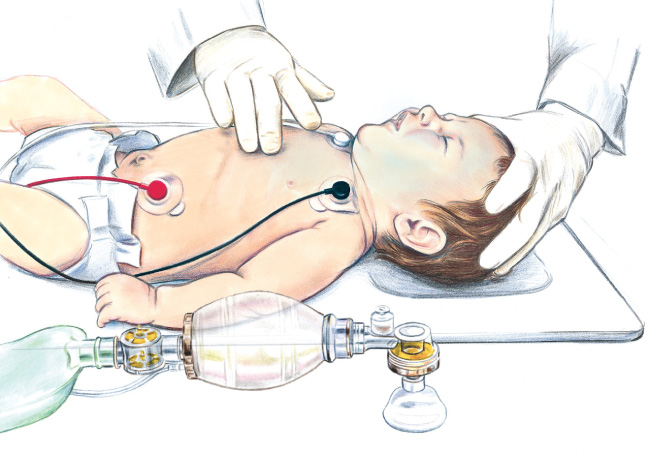
2. Hand Placement and Compression Technique:
When performing pediatric CPR on children above the age of one year, hand placement remains relatively similar to adult techniques. The caregiver should position themselves beside or slightly above the child's chest and place their hand at the centre of their chest on the lower half of their breastbone (sternum). However, when performing compressions on infants under the age of one year old, it's important to remember that they have a smaller chest cavity and more delicate bones. Caregivers should use two fingers rather than their entire hand for compression.
3. Adjusting Compression Depth and Rate:
Adjusting both compression depth and rate is crucial to ensure effective CPR in young individuals. Adult guidelines recommend compressions with a minimum depth of two inches (5 cm). But when dealing with pediatric cases, partial sternum depression up to 1/3 or approximately 1½ inches deep (4 cm) is preferred. In terms of compression rate, it is vital to maintain a steady pace of at least 100 compressions per minute for both adult and pediatric cases.
4. Modifications for Infants:
Pediatric CPR guidelines should also address the unique needs of infants under the age of one, particularly newborns. When providing CPR to a newborn, lay the infant on a firm surface and make sure the head remains in line with the body. Since their airways are tiny and more delicate than those of older children or adults, it's important to use gentle taps rather than strong back blows or head tilts when performing airway clearance techniques.
5. Dealing with Choking Hazards:
Choking emergencies can happen to individuals of any age group but are a common concern when dealing with young children and infants who often tend to put foreign objects into their mouths. For pediatric cases (children aged 1 to puberty), the Heimlich maneuver is usually recommended for choking incidents caused by solid objects lodged in their airways. However, for infants under one year, caregivers may need to use back blows followed by chest thrusts instead.
6. Proper Rescue Breathing Techniques:
In addition to performing chest compressions, rescue breaths are an integral part of pediatric CPR. While the compression-to-breath ratio changes compared to adult CPR, it is essential to ensure that rescue breaths are performed correctly for optimal results. When providing rescue breaths to children above one year old, each breath should be delivered over approximately 1 second. Use a seal by opening their airway with a head tilt and chin lift and placing your mouth over their nose and mouth securely. For infants under one year, perform gentle puffs of air into their nose and mouth instead.
Conclusion
When it comes to pediatric CPR, adapting techniques for younger individuals is crucial in order to maximise the chances of recovery during an emergency situation. By understanding the key differences between adult and pediatric CPR approaches and knowing how to adjust hand placement, compression depth, and rate, as well as addressing specific challenges like clearing airways or handling choking hazards peculiar to infant stages, caregivers can play a vital role in saving lives.
Remember that obtaining proper certifications, participating in regular refresher courses, and familiarising yourself with recommended guidelines from credible organisations like the American Heart Association (AHA) or American Red Cross are essential in maintaining an accurate knowledge base on pediatric CPR techniques. By doing so, you can have confidence in your ability to respond effectively during life-threatening situations involving young individuals.









